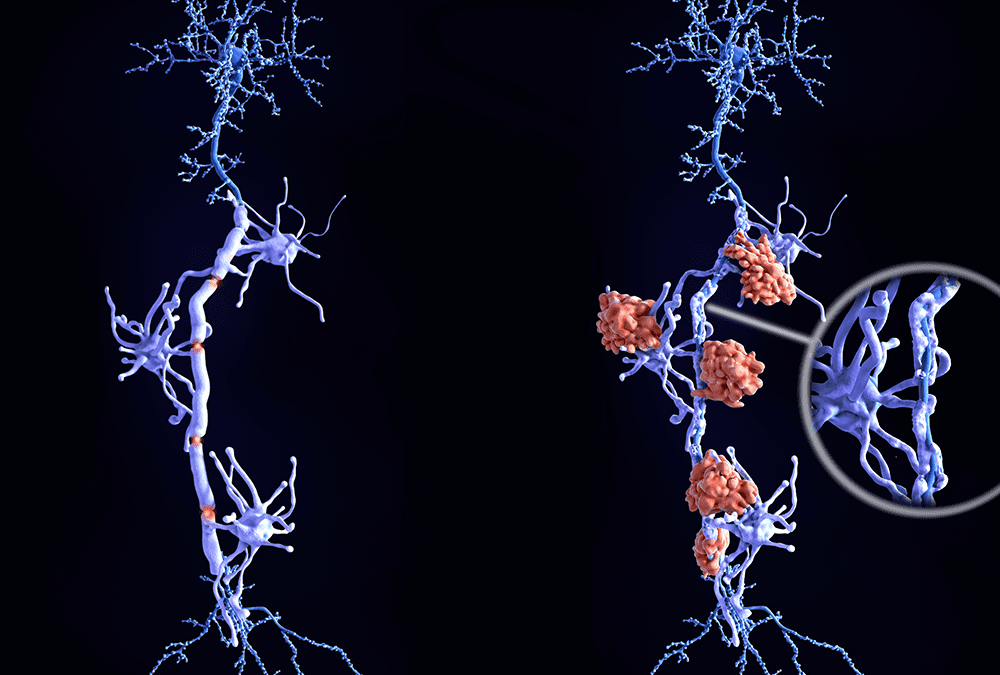
Progressive multifocal leukoencephalopathy (PML) is a rare but devastating neurological disease that affects the immunosuppressed population. The etiologic agent is a polyomavirus, JC virus – a double stranded DNA virus with a high prevalence of infection globally. PML is believed to occur from reactivation of the latent virus infection caused by immunosuppression. After 1980, a dramatic increase in the incidence and prevalence of PML was attributed to the HIV/AIDS pandemic, with a decline noted after the introduction of highly active antiretroviral treatment (HAART). Newer populations are being added to the risk pool for the development of PML with the introduction of biologic agents that target specific arms of the immune system.
In a report, The Changing Landscape of Progressive Multifocal Leukoencephalopathy, (Current Infectious Disease Reports. 2011 May 21), Kedar S, Berger JR. of the University of Kentucky reviews current literature on the pathogenesis of PML with a focus on development and risks.
Based on the review of PML pathogenesis literature regarding the epidemiology of the JC virus (JCV), conditions that predispose to PML (a focus on AIDS), medications that increase the risk of PML (i.e. natalizumab [TYSABRI], efalizumab [Raptiva], rituximab [Rituxan], belatacept, alemtuzumab, and mycophenolate mofetil [CellCept]), and potential risk mitigation strategies, the main findings are:
1. The precise mechanism through which JCV causes PML is unknown.
2. The exact mechanism through which medication increases the risk of PML remains to be uncovered.
Additionally, PML is hypothesized to be the result of a complex interaction between host and viral factors; and further research is needed to understand the mechanisms responsible for the development of PML.
While studies using other assays have demonstrated a large variability in anti-JCV antibody prevalence, studies in MS patients using the Biogen Idec/Elan anti-JCV antibody assay, irrespective of treatment, have demonstrated an approximate 55% anti-JCV antibody prevalence. As such, the authors suggest that re-testing for anti-JCV antibodies every 6 months may be necessary.
As more patients are treated with these agents, risk mitigation strategies have been developed to prevent PML.

Specializing in rare disease, Boston Biotech Clinical Research works with biotech, pharmaceutical, device companies and investors to streamline the clinical trial process. Our experienced team helps each client reach their specific goals by customizing a clinical and regulatory road map of simplified programs and streamlined protocols to meet our clients’ requirements.